Grand Opening of Hometown Veterinary Partners in Naperville
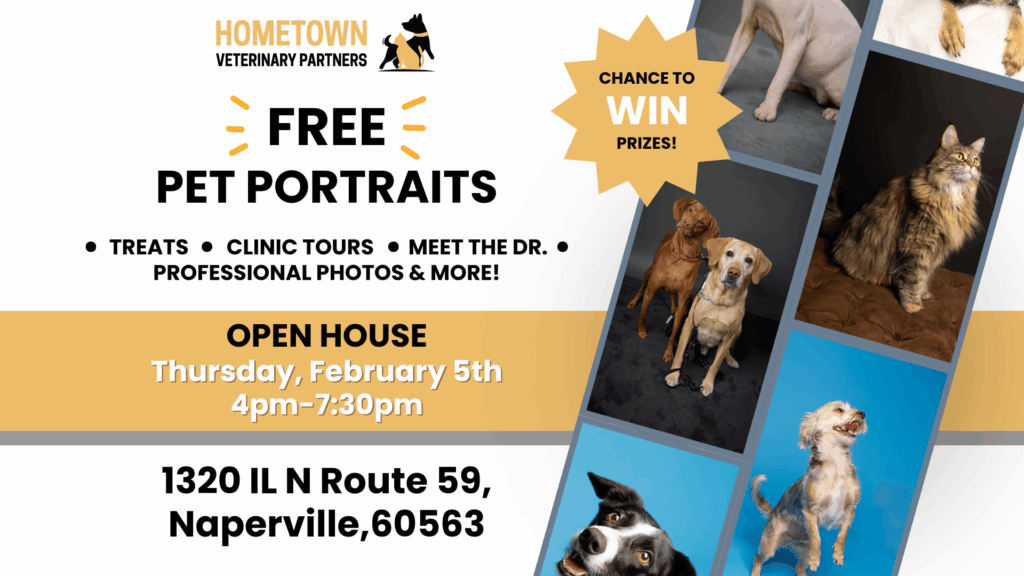
We’re Opening Our Doors in Naperville—Join Us for the Grand Opening Celebration! Big news, Naperville—we’re officially opening our doors! Hometown Veterinary Partners of Naperville is excited to invite the community to our Grand Opening celebration on Thursday, February 5th from 4:00–7:30 PM. This special evening marks the launch of our newest location and is our […]
5 Pet Stocking Stuffers for Cats and Dogs

Holiday Gift Guide from Your Hometown Veterinary Team The holidays are here, which means twinkly lights, cozy evenings, and the perfect excuse to spoil the furry members of the family. If you’re building a stocking for your pet this year, we’ve rounded up safe, vet-approved gift ideas that bring joy without the hazards. We’ve included […]
From Dairy Science to Small Animal Care — Meet Dr. Colbi Carr
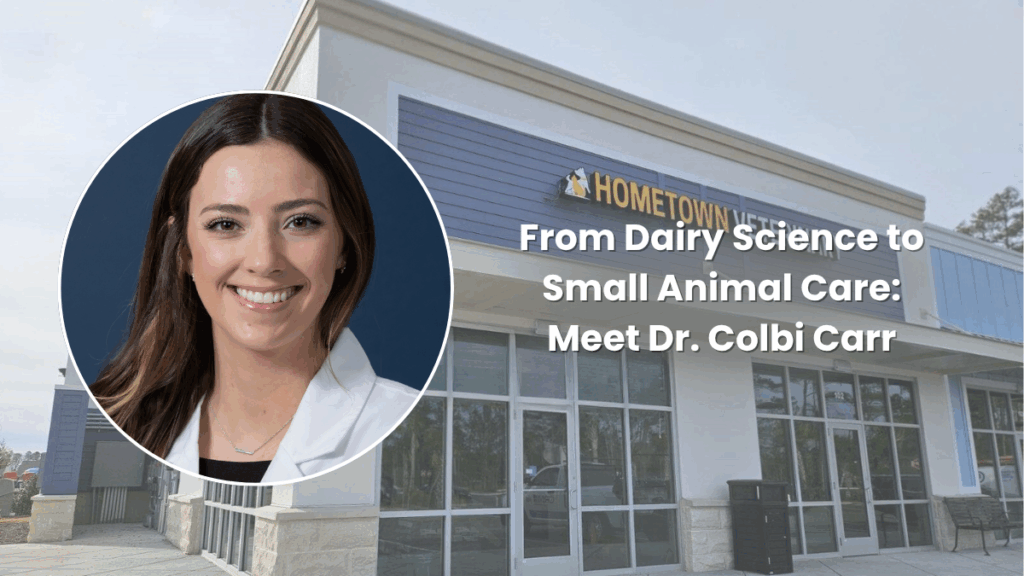
Hometown Veterinary Partners is thrilled to welcome Dr. Colbi Carr to our Myrtle Beach team! Dr. Carr’s path to veterinary medicine began long before she ever put on a white coat. Growing up surrounded by animals—from family dogs and a cat in a play stroller to her grandparents’ chickens, she discovered early on that her […]
Grand Opening of Hometown Veterinary Partners in St. Louis

We’re excited to announce the Grand Opening of our brand-new Crestwood clinic, and you’re invited to celebrate with us! Join us on Saturday, October 11th from 11 AM – 3 PM at 9575 Watson Rd, St. Louis for a day full of fun, pets, and community. What to Expect Ribbon Cutting with the Chamber of […]
Meet Dr. Diaphni Taylhardat: Compassion, Experience, and a Heart for Pets
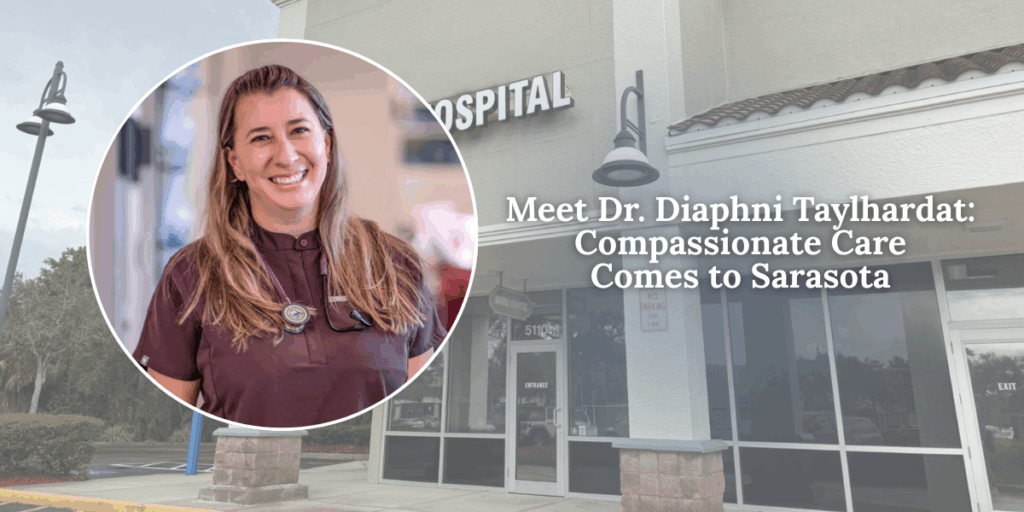
With more than 17 years of veterinary experience, Dr. Diaphni Taylhardat brings an incredible blend of knowledge, compassion, and dedication to every patient she cares for. Her journey in veterinary medicine began at the Central University of Venezuela, where she earned her degree and discovered her lifelong passion for helping animals. A Diverse Background in […]
Meet Dr. Delaney Rohan: Compassionate Veterinary Care Close to Home
Looking for a veterinarian in North Saint Paul who treats your pet like family? Meet Dr. Delaney Rohan, one of the newest and most compassionate members of our team at Hometown Veterinary Partners. A Lifelong Passion for Helping Animals Dr. Rohan has always known she wanted to be a voice for animals. Her journey into […]
Why Year-Round Flea & Tick Prevention Is a Must for Every Pet

Why Year-Round Flea & Tick Prevention Is a Must for Every Pet Fleas and ticks may be small, but the problems they cause can be huge. These parasites don’t just irritate your pet—they can carry serious diseases, lead to infections, and cause lasting health complications if left untreated. That’s why year-round flea and tick prevention […]
A New Chapter for Best Friends Animal Hospital – Sarasota
A New Chapter for Best Friends Animal Hospital – Sarasota We’re thrilled to announce that Best Friends Animal Hospital in Sarasota is now part of the Hometown Veterinary Partners. This partnership marks the beginning of an exciting new chapter—one grounded in a shared commitment to exceptional, compassionate care for pets and the people who love […]
Meet Dr. Longtin: Compassionate Veterinary Care Rooted in Experience and Heart

Caring for animals isn’t just what Dr. Longtin does—it’s who she is. With nearly 30 years of experience caring for pets and their people, Dr. Longtin brings a wealth of knowledge, empathy, and a deeply personal approach to every appointment. A proud graduate of the University of Minnesota College of Veterinary Medicine, she’s spent her […]
Dr. Cheryl Brocki Joins Hometown Veterinary Partners as Chief Veterinary Officer

Hometown Veterinary Partners is proud to announce the addition of Dr. Cheryl Brocki as our new Chief Veterinary Officer (CVO). With an extensive background in veterinary operations, mentorship, and clinical excellence, Dr. Cheryl Brocki joins our executive leadership team at an exciting time in our growth. She will play a key role in shaping the […]

















